Week 3 - Introduction to health policy, issues
Introduction to healthcare, health policy, and healthcare economics; objectives of HP; concepts, measurement; policy issues.
Study literature
The main concepts, relations, and issues are well explained in the following study. Please spend your time during the semester reading it.
Summary of the Week 3 Lecture
1. Analyzing health policy - what does it mean?
Policymaking includes at least four core dimensions (Walt and Gilson, 1994):
- content (goals, priorities, measures);
- context (values, path dependence, economic and social conditions, issues);
- process (agenda setting, negotiation, lawmaking, implementation); and
- actors (institutional, informal, leaders, power groups...).
2. Why Public - Why Government?
Public policy = an expression of strong interest. There is an active and strong government's role in the provision, organization, and funding of healthcare/medical services in literally all developed countries. Why it is for?
Besides the most relevant social arguments (equity, fairness, humanity, specific egalitarianism), the health economics theory (for example Feldstein, 1993) also points at some efficiency issues – “market failures” connected with health care delivery. From the point of view of allocative efficiency, several obstacles prevent the achievement of allocative efficiency in the health-care market, primarily:
- informational asymmetry;
- externalities; and
- uncertainty and complexity.
The absolute classics here is Kenneth Arrow's article Uncertainty and the Welfare Economics of Medical Care (1963). It's really a "must-read" for anyone who wants to understand the context.
References:
- Walt, G. & Gilson, L. (1994). Reforming the health sector in developing countries: the central role of policy analysis. Health Policy and Planning. 9, 353–70.
- Feldstein, P. (1993). Health Care Economics. Albany: Delmar Publishers.
Values, Assessment criteria
Equity, Access, Availability, Quality, Effectiveness.
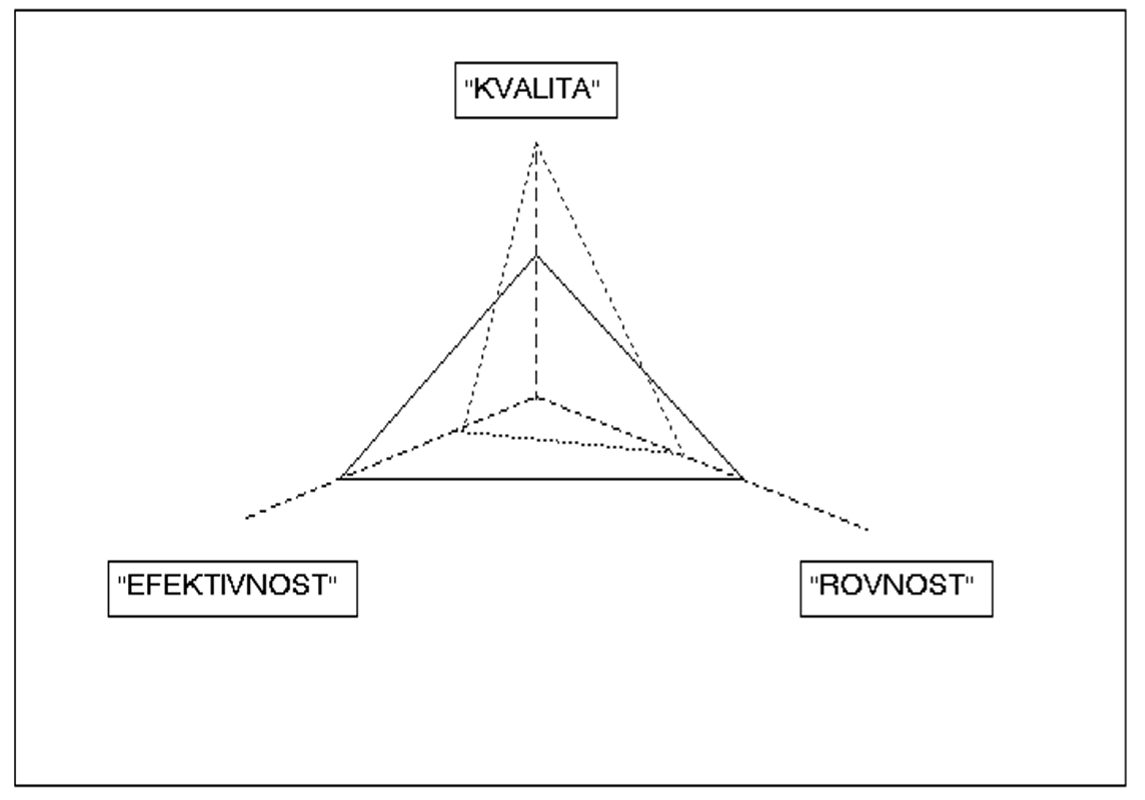
"Magical triangle"
Equity - one of the most relevant values connected to health care provision.
According to Kendall & Knapp (2000), equity is fairness or justice and is usually discussed in relation to the enjoyment of effects or benefits (intermediate or final outcomes), and/or the burden of paying for them. Equity assessments thus pose questions such as: Do people with equivalent needs have access to, or use equivalent amounts of, certain goods or services? Do people with greater needs get more services? Do people with greater means (for example, in relation to income, wealth, innate abilities or opportunities) contribute disproportionately more to the costs of producing collective goods or services? Alternatively, is it right that better-off members of the community should have to pay more (through taxes, say) than worse-off members, even when the latter make greater use of services funded out of taxation?
The concept of equity in relation to health and health care can mean different things to different people. What Whitehead's discussion paper has tried to do is to pin down some of the essential elements by pointing out not only what we are aiming for, but also what we are not aiming for. Equity does not mean that everyone should have the same health status, for example, or consume the same amount of health service resources irrespective of need. Some people may dismiss the goal of equity altogether if they interpret it along such lines.
For details please check these two documents: