Female reproductive system
A reproduction system is a set of organs aimed at sexual reproduction. Its basic function is the production of sexual cells and the transfer of genetic information to offspring. Unlike other organ systems, the organs of the reproductive system are sexually different. The primary genitals are the gonads producing sexual cells, ovaries in women and testicles in males. These glands also produce sexual hormones, with testosterone forming in the testes, and estrogen and progesterone in the ovaries. The reproductive system consists of other glands and organs involved in the reproduction.
Although men can practice hormonal yoga, they are very sporadic in classes. Hormonal yoga is mainly popularised among women and practised by them. Therefore, this chapter deals with the female reproductive system.
Menstrual cycle
The menstrual cycle is a basic and very important process in terms of reproduction. It is a programmed, cyclically repetitive process controlled by the hormones of the hypothalamic-pituitary system and the ovaries. The environment, nutrition and the state of the organism can also influence its course and regularity. The first menstrual bleeding occurs in girls between the age of 12-16. After women reach 40, the cycle becomes irregular, with the transition period lasting up to 10 years. At the age of 48-52, the last bleeding and menopause usually occur.
The menstrual cycle usually lasts 28 (21-35) days. If the cycle is irregular with deviations greater than 2-3 days, the ovulation does not have to occur, which is about 20% of all cycles in a healthy woman.
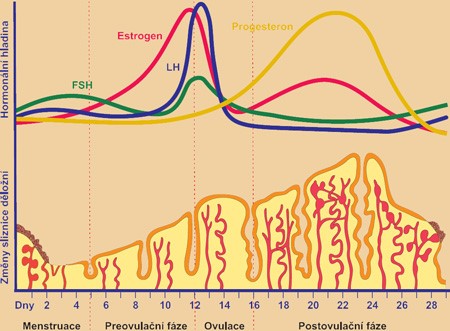
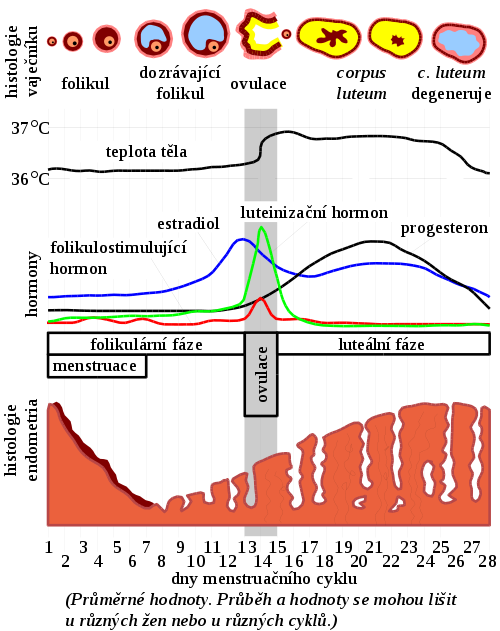
The mestrual cycle is divided into several phases:
- Phase 1 – menstrual bleeding occurs in the menstrual phase, which lasts for 2 to 7 days. The average blood loss is 35-45 (20-80) ml. In the uterus, the blood vessels constrict for several hours, and unnecessary cells of the endometrium die. After releasing the constriction, new blood flows into the endometrium sweeping away these dead cells. The body gets rid of all unnecessary components, unimpregnated eggs, old and dead cells of the endometrium together with blood and mucus.
- Phase 2 – in the follicular (proliferation) phase, which lasts for about 6 days, one egg cell matures in a follicle, new soft cells of the endometrium grow, the cervix begins to produce more mucus, then it opens and shortens.
- Phase 3 – in the ovulation phase, within the first 2-3 days the matured egg cell is released into the fallopian tube. The watery and elastic cervical mucus maintains an alkaline environment in the vagina and helps a sperm reach an egg. If the egg is not impregnated within about 12 hours after it is released, the egg disintegrates. After the egg is released, the low basal temperature increases.
- Phase 4 – in the secretory (luteal) phase, the empty follicle is transformed into a corpus luteum, and the endometrium grows. The amount of cervical mucus is reduced and becomes more dense and acidic. If the egg was not impregnated, the yellow body turns into a corpus albicans. The blood vessels of the endometrium start to constrict and its cells begin to die gradually.
Hormones of the menstrual cycle
The hormones involved in controlling the menstrual cycle include gonadorelin (gonadoliberin (GnRH)), two gonadotrophins: follicle-stimulating hormone (follitropin (FSH)) and the luteinizing hormone (lutropin (LH)), as well as oestrogens (E) a progesterone (P) – see picture 1.
Gonadorelin (luliberin) is a hormone responsible for the production of the luteinizing hormone and the follicle-stimulating hormone in the pituitary gland. Gonadorelin is synthesized and released inside the hypothalamus.
Gonadotropins (follitropin and lutropin) are two hormones of the anterior lobe of the pituitary gland. They control the activity of the sex glands, and regulate the production of the sex hormones, estrogen and progestin, and the maturation of sex cells.
Estrogens are produced in the ovaries, in the corpus luteum and placenta. The liver, suprarenal glands and breasts also produce a small amount of estrogen, which is important for postmenopausal women. The level of estrogen is at its highest at the end of the follicular phase, the peak directly preceding ovulation. The most important and most effective of the group of estrogens is estradiol (E2) produced in the corpus luteum in the ovaries. Other estrogens include estrone (E1) produced by the ovaries, adrenals and fatty tissue and estriol (E3) produced by the placenta. Estron and estriol have a significantly weaker efficacy than estradiol. Estrogens induce the proliferation phase of the menstrual cycle and stimulate the secretion of the sparse mucus in the uterine cervix. They are responsible for the development of female sexual characteristics and for the optimization of the effects of progesterone. They support the follicular maturation and have a negative feedback on the secretion of the luteinizing and follicle-stimulating hormones at physiological levels. At very high levels, however, they impart a positive feedback on these hormones.
Progesterone is made of cholesterol in the corpus luteum of the ovaries and in the suprarenal glands. Progesterone is the best-known hormone of progestins whose levels rise just before the ovulation with the peak reached 5-7 days before it. The task of progesterone is to prepare and maintain the endometrium for and during pregnancy. It introduces the secretory phase of the menstrual cycle, supports the growth of the endometrium after ovulation. It is responsible for muscle reconstruction, for the supply of vessels in the uterus, for maintaining the secretory phase in it to be prepared for nursing the egg. Progesterone inhibits the release of the luteinizing hormone in the luteal phase. Its administration in the follicular phase suppresses the ovulation, which, along with other factors, is the basis of the contraceptive pills.
Hormonal regulation of the menstrual cycle
Because the objective of hormonal yoga is the harmonization of hormonal levels in a human body, it is advisable to understand all these processes. This subchapter therefore details the hormonal processes during the menstrual cycle.
Hormonal regulation of the menstrual cycle – Schematic depiction
At the end of the luteal phase and at the beginning of the follicular phase, the level of the luteinizing hormone (LH) is relatively low and there is a gradual increase in the secretion of the follicle-stimulating hormone (FSH). Due to the follicle-stimulating hormone, the follicles mature in the ovaries, and one of them starts to produce estrogen (E). This secretion is the highest and most important during the first week of the follicular phase of the menstrual cycle. At the end of the follicular phase, the level of follicle-stimulating and luteinizing hormones increases. The high level of the follicle-stimulating hormone induces the first egg cell division and the secretion of estrogens and progesterone in the ovaries by activating the enzyme aromatase and p450 enzymes. It also influences the secretion of gonadoliberin (GnRH) by negative feedback.
The rapid increase in estrogens in the follicle results in an increased secretion of the luteinizing hormone from the anterior lobe of the pituitary gland, producing more androgens and more estrogens. The luteinizing hormone is vital for the growth of pre-ovulation follicles as well as for the ovulation of the dominant follicle and subsequent luteinization, i.e. the conversion of a matured follicle in the ovary into the corpus luteum after the ovulation. About 10 hours later, the level of the luteinizing hormone reaches its peak, the dominant follicle bursts, the egg is released, and the ovulation starts. Unless this sudden rise in the luteinizing hormone occurs, the ovulation does not occur and pregnancy is not possible.
At the beginning of the luteal phase, the luteinizing hormone, follicle-stimulating hormone and estrogens cause the conversion of the follicle into the corpus luteum producing the progesterone and a small amount of estrogen. The estrogen and progesterone suppress the secretion of the follicle-stimulating and luteinizing hormones (partly indirectly by the inhibition of gonadoliberin), whose concentration in the plasma decreases. Through this negative feedback, when the levels of estrogen and progesterone decrease, menstrual bleeding occurs. At the same time, there is a gradual increase in the follicle-stimulating hormone. The menstrual cycle starts with menstruation at the beginning of the follicular phase. The follicular phase ends with ovulation, which goes into the luteal phase.
The increased level of the follicle-stimulating hormone stimulates the follicular secretion of estradiol. On the granulosa cells (i.e. supporting cells which create the cover of immature egg cells), the expression of the aromatase receptors increases the convertion of androgens into estrogens. The follicle-stimulating hormone simultaneously induces the expression of follicle-stimulating hormone receptors on the follicles. This enhances the effect of the follicle-stimulating hormone and the follicles produce more extradiol. The estradiol level peak occurs on the 10th-13th day of the menstrual cycle before ovulation.
An increased level of estradiol initially causes negative feedback on the anterior lobe of the pituitary, thus diminishing the secretion of the follicle-stimulating and luteinizing hormone. Their level decreases between the 11th and 13th day of the menstrual cycle. The level of estradiol peaks and the feedback changes to positive, resulting in the pre-ovulatory release of the luteinizing and, to a lesser extent, folliculostimulatory hormone.
The release of the luteinizing hormone iniciates the process of ovulation (egg release) and luteinization, or, to put it differently, the transformation of the follicle (the remaining granulosa cells, the cover of the follicle, and the remaining connective tissue) to the corpus luteum. After luteinization, the granulosa cells begin to produce progesterone instead of androgens, the expression of the the luteinizing hormone receptor increases in these cells, and the affinity for the estrogen and follicle-stimulating hormone decreases. The progesterone secretion peaks between the 5th and 7th day after the ovulation.
Progesterone and estrogens are produced by the corpus luteum and their secretion increases until the yellow?? corpus luteum begins to degenerate during the luteal phase. The production of progesterone is significantly higher than the production of estrogen and reaches its peak. The level of estrogen decreases, the corpus luteum degenerates into the corpus albicans. The production of progestone and estrogens decreases and hormone levels decline.
The decrease in the hormone levels of progesterone and estrogen no longer induces negative feedback at the pituitary level. The secretion of the follicle-stimulating hormone stops being inhibited and starts rising again, which results in menstruation.
If the egg is not impregnanted and its nesting does not occur, the secretion of gonadoliberin is inhibited by progesterone and estrogens on the 22nd day. The corpus luteum is transformed and ceases to produce hormones. This rapid decline results in the constriction of the blood vessels in the uterus, the cells of the endometrium begin to decouple, and menstrual bleeding occurs. If the egg is not fertilized, it perishes and the rests of the Graaf's follicle changes from the corpus luteum into corpus albicans.
Sexual maturity
Sexual maturity is the state when women can reproduce. Then, a secretion of gonadorelin begins in the hypothalamus, stimulating the production of the follicle-stimulating and luteinizing hormone in the hypophysis. The secretion of gonadorelin occurs in pulses, which is one of the preconditions for a normal menstrual cycle. The average frequency of this secretion is once in a 90-minute period during the early follicular phase, increasing up to once a 60-70-minute interval later in the follicular phase. During the luteal phase, the frequency decreases to once a 4-5-hour interval, but the amount of produced hormone increases. This induces a pulsatile release of the follicle-stimulating and luteinizing hormone from the adenohypophysis. Any disorders of this rhythm, an acceleration or continuous distribution, decrease the secretion of the follicle-stimulating and luteinizing hormone and result in a possible subsequent infertility. The follicle-stimulating and luteinizing hormones subsequently regulate the production of estrogen and progesterone. Many psychological factors and stress can influence the secretion of both these hormones. All these factors reduce both their production and the production of sexual hormones in the ovaries. The ovarian hormones then indirectly affect the production of gonadorelin.
Menopause
The menopause is a period of time when women stop menstruating. It is a natural period when the activity of the ovarian falls and the production of estrogen and progesterone decreases. The menstrual cycle disappears, and the period of natural infertility starts. Menopause begins in women aged 45 to 55, but there may be deviations in the age. From the medical point of view, the menopause means the absence of menstruation for longer than one year. Perimenopause usualy precedes the menopause, characterized by irregular menstrual bleeding. Perimenopause usualy affects women for four years before the menstrual bleeding completely disappears. Various inconveniences, difficulties and troubles may accompany the menopause. However, not every woman has to undergo these unpleasantnesses. Positive attitudes to life, positive thinking, and care about physical and mental health may decrease these symptoms in acitve women.