Pigmented lesions of the oral mucosa caused by exogenous pigmentations were described in the Chapter 5.2.4. In endogenous pigmentations, the pigment is formed in the organism itself; such pigments include in particular melanin, hemosiderin, ferritin, porphyrin precursors and discolorations of vascular origin (Fig. 10).

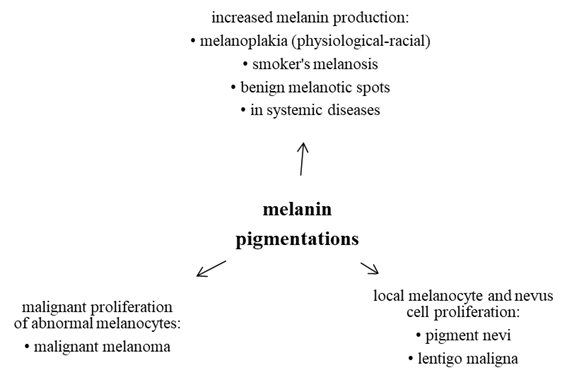
Melanocytes of the oral mucosa usually do not produce melanin as their activity is stimulated by the exposure to UV irradiation; other stimulants of their activity include oestrogens (manifestations on the skin and lips such as chloasma gravidarum during pregnancy), mechanical or chemical irritation (reactive posttraumatic or postinflammatory hyperpigmentation), smoking (smoker’s melanosis) and some drugs. Melanin pigmentations of the oral cavity can be physiological (racial, freckles - ephelides) or pathological that may clinically manifest as solitary, diffuse or multiple. They are most commonly formed as a result of increased melanin production by melanocytes. Other possibilities include local proliferation of melanocytes and nevus cells; malignant proliferation of abnormal melanocytes is the worst scenario (Fig. 11).
It occurs in some smokers, probably as a defensive reaction of the organism against smoking. Chemical and thermal irritation stimulate the production of melanin that can protect the mucosa by binding the toxic compounds and prevent their penetration into deeper layers. It is especially common on the gingival, buccal and palatal mucosa. After smoking cessation, it can regress spontaneously
Oral and labial melanotic macules are caused by hyperproduction of melanin in the basal layer of the mucosa. They are usually solitary but can be multiple, usually well circumscribed, they can develop suddenly and remain stable and stationary. They can be found in adults, most commonly in the vermilion zone, gingiva, buccal and labial mucosa (but they can develop even on genitals).
Oral melanoacanthoma is a reactive hyperpigmentation developing as a result of a mild injury or chronic irritation.
Melanin pigmentations appear in Addison’s disease, Peutz-Jeghers syndrome, bronchogenic pulmonary carcinoma and other tumours, or in acanthosis nigricans.
In the primary form of the adrenal hypofunction caused by a damage to the adrenal cortex, the systemic symptoms (hypotension, disorders in electrolyte metabolism) can be accompanied by diffuse hyperpigmentation (so-called “bronze skin” or hyperpigmentations in the genital region and in the areolas) and/or by greyish-black focal pigmentations (so-called graphite stains) on the oral mucosa, especially on the buccal mucosa in the region of the molars and on the sides of the tongue. The increased pigmentation, especially in the areas of increased mechanical irritation, are caused by an increased pituitary production of the adrenocorticotropic hormone (ACTH) and melanocyte stimulating hormone (MSH) or, rather, of their common precursor, pro opiomelanocortin. In secondary insufficiency of the adrenals (i.e., if hypothalamus or pituitary gland are affected), such hyperpigmentation does not occur.
Some malignancies can result in melanotic changes on the palate that arise by a mechanism similar to that found in Addison’s disease, i.e., as an effect of the formation of a common precursor of ACTH and MSH.
This autosomal dominant hereditary disease counting among hereditary tumour syndromes affects both sexes with the same frequency. It is a hamartomatous polyposis of the gastrointestinal tract (most commonly affecting the colon), accompanied with mucocutaneous, in particular oral, hyperpigmentations. Those melanotic (dark brown) spots are well circumscribed and located most commonly near the body openings – in the face, it is in particular on the lids, around the nostrils, circumorally, sometimes on the vermilion, or on the labial, buccal, lingual or palatal mucosa. Polyps in the GIT can cause sudden gastric/abdominal colics or GIT bleeding. An increased tendency to developing carcinomas of the GIT, uterus, ovaries, breasts and testicles are the reason for classifying this syndrome as precancerosis and mucocutaneous paraneoplasia.
This papillomatous-verrucous focal, melanin-pigmented disease of the skin or mucosa can occur either in a benign or malignant form.
The benign form can be categorized as follows:
Malignant acanthosis nigricans has a character of a paraneoplastic process and can occur with tumours of the stomach and colon. For diagnostic purposes, it is necessary to note that it can precede the manifestation of the tumour by up to a year. Lesions on the face are usually symmetrical, lips are often affected as well as the tongue (macroglossia can be present) and the buccal mucosa. Lesions have indistinct edges, mostly flat with rough surface. Similar lesions can occur on other mucosal surfaces (e.g. on the conjunctiva or rectum).
Pigment nevi are not common on the lips and oral mucosa. They can occur in children but their peak is in the 3rd-4th decades of life. They can be of various colours (blue, brown, black; even the amelanotic form is possible). They are usually solitary, well circumscribed, flat or elevated, several millimetres large and do not change over time. A pigment nevus goes through several stages of development: junctional, compound and intramucosal. Unlike melanin pigmentations caused by an elevated production of melanin, pigment nevi arise as a result of melanocyte proliferation and their transformation into nevus cells. Some types of pigment nevi can be potential precursors of the development of the malignant melanoma.
Dg.: Verification by histology
Th.: Surgical
This special type of pigmented nevus always transforms into malignant melanoma. It only rarely develops in the area of the lips and oral mucosa. If so, a typical manifestation (usually on the palate or lower alveolus) is a dark, central melanotic spot with smaller satellite lesions that can be sometimes of a different colour, with diffuse edges and quickly changing appearance.
Dg.: Like in the case of the malignant melanoma, can only be verified histologically.
Th.: Surgical.
Occurrence of the melanoma in the oral cavity is rare (approx. 1 % of all malignant tumours of the oral cavity). It almost always occurs on the palate or the alveolar ridge of the maxilla in patients of higher age, it is more common in males. It develops either by malignant transformation of a pre existing pigmented lesion or „de novo“. Typical symptoms include a sudden development, rapid growth (weeks to months), invasion into the surrounding tissues, tough consistence and, frequently, ulcerations of the existing melanocytic lesion.
Dg.: Must be made by a pathologist based on morphological characteristic of a bioptic sample.
Th.: Surgical, the excision must have a sufficiently wide resection margin.
This rare autosomal recessive disease is characterised by excessive absorption and pathological deposition of Fe in the organism. It affects in particular middle-aged males. The clinical picture includes cutaneous and oral mucosal hyperpigmentations with dark bronze reddish-brownish hue resulting from deposition of the haemosiderin and haemofuscin pigments. Hepatomegaly is often present, as well as hepatic cirrhosis (leading to development of a hepatoma in about 25 % of patients) and diabetes mellitus (so-called „bronze diabetes“).
This term refers to a group of disorders associated with porphyrin metabolism, namely with excessive production of porphyrins and their precursors (haemoglobin, biliverdin, bilirubin). Each type of the disease is characterized by a defect of a specific enzyme involved in the haem synthesis. According to the tissue where the abnormal synthesis of porphyrins takes place, porphyrias can be classified into 3 categories (with many subcategories): erythropoietic, hepatic and mixed. Typically, the skin is very photosensitive and abnormally fragile with erythema, vesicles or even bullae, erosions, hyperpigmentation and hypertrichosis. The oral mucosa is affected less often; cinnabar-coloured lesions can form on the lips, corners of the mouth, vestibular and gingival mucosa.
Such discolorations are caused by small dot-like (petechiae, purpura) or larger (ecchymoses, haematomas) bleeding into the tissues caused by injury (e.g. biting), bleeding disorders or due to multiplication/dilation of vessels/capillaries (teleangiectasia, sublingual venectasia, haemangioma). Rarely, such discolorations can be also caused by malignant vascular proliferation (angiosarcoma-Kaposi’s sarcoma). Unlike the melanin-associated pigmentation, pigmentations of vascular origin are of red-blue-Bordeaux colour.